Part One of a Two-Part Series on Psychedelics and Chronic Pain
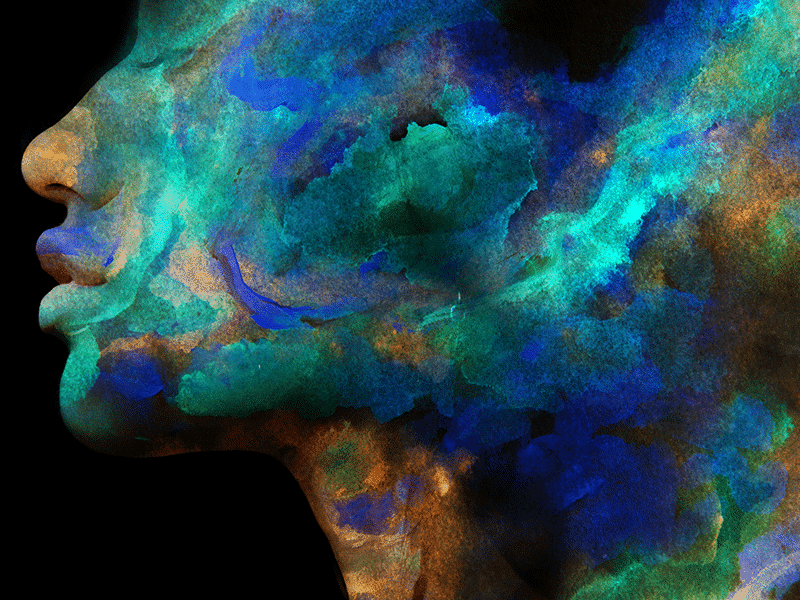
The key is neuroplasticity: the brain’s ability to change and adapt (or, as is often said in psychedelic circles, to rewire itself) such that negative or harmful patterns of thought are disrupted, and new, healthier paths are forged in their place.
This is the general mechanism through which scientists now believe at least some of the benefits of psychedelics for a wide range of psychiatric disorders occur. And in much the same way that they appear to help treat depression, addiction, post-traumatic stress disorder, obsessive-compulsive disorder, and other mental-health conditions, psychedelic drugs are now being investigated as a remedy for a particularly troublesome form of chronic pain.
Neuroplasticity appears to play a central role in the published case study of a 35-year-old man whose intractable phantom-limb pain resulting from an amputated leg suddenly all but disappeared. The treatment? Three doses of psilocybin paired with mirror visual feedback. a form of therapy used to relieve amputee phantom-limb pain in which patients position a mirror in the middle of their body and perform a motor task with one limb while watching its reflection, giving the illusion of the missing limb moving.
Not Just a Lot of Good Vibes
The article describing this rapid recovery aided by psilocybin mushrooms was published in the journal Neurocase in May 2018 and co-authored by the patient himself, one Albert Lin, a research scientist at the University of California at San Diego (UCSD) and National Geographic explorer and television host. Four of Lin’s colleagues at UCSD, including neuroscientist Vilayanur Ramachandran, who pioneered mirror visual feedback in the early 1990s, also contributed to the article.
While they are certain that this combination of high doses of the psychedelic compound and mirror visual feedback caused Lin to no longer feel sharp pain in his missing foot, the authors admit they are not entirely sure how that happened. One theory, and a highly plausible one at that, is grounded in what we already know about how the classic psychedelics – those whose efficacy centers on activation of the 5-HT2A serotonin receptor – literally help the brain make new connections.
“It is possible that the psychoactive effects of psilocybin are accompanied by an increased state of cross-modal functional connection and neuroplasticity via serotoninergic effect,” the authors speculate. “If this is the case, then the psilocybin might both make the brain more receptive to mirror therapy and make the pain reduction last longer or even disappear.”
In other words, the drug and the therapy appear to have worked together to rewire Lin’s mind. The outcome was both lifesaving for this “bionic Indie Jones” – who now surfs, swims, and hikes with his prosthetic leg – and illuminative of the power of psilocybin and neuroplasticity. (Still, perhaps to avoid mentioning magic mushrooms, a profile of Lin in The San Diego Union-Tribune chalked his healing up to “a whole lot of good vibes.”)
A New Clinical Trial
Two years after Lin’s case report was published, another paper from UCSD researchers further probed the link between psychedelics and chronic pain. This was primarily a review article, with no new data, but it did gather together in one place all of the existing evidence in the scientific literature for the treatment of various forms of chronic pain with psychedelics, specifically psilocybin and LSD. In all, it turned up only eight papers dating as far back as 1964.
Among these, two others dealt with phantom-limb pain. The first, from 1967, contained more case studies. Five of six patients profiled in the paper achieved significant and sustained reduction in phantom-limb pain following the use of LSD. The second, from 1977, described how five of seven phantom-limb pain sufferers saw an improvement in pain and at least a 50% reduction in the use of painkillers after taking LSD.
Now, some of the authors of that review are seeking to add to the evidence base through a new clinical trial. Housed within UCSD’s Psychedelics and Health Research Institute – formed in 2016 following, and inspired by, Lin’s rehabilitation – the study will be the world’s first randomized, placebo-controlled human clinical trial examining the safety and efficacy of treating chronic phantom-limb pain with psilocybin.
The research team hopes to begin enrolling a total of 30 patients by the end of summer. Half will receive a relatively large dose of psilocybin (25mg) on two occasions, and the other half will see two doses of niacin, a placebo. The researchers will use magnetic resonance imaging to look for brain changes post-dosing, then correlate these findings with measures of pain and psychological functioning assessed on subsequent clinical visits.
Approximately 1.7 million people live with limb loss each year in the United States, and the vast majority experience phantom-limb sensations beginning in the days and weeks after amputation. For many, the pain can be severe and difficult to treat using existing therapies. That was certainly the case for Lin, who tried opioids, cannabis, and the nerve pain medicine Pregabalin before experimenting with psilocybin. Though the new trial won’t include mirror visual feedback, its success could still point toward a potentially life-altering new option for millions who suffer from this debilitating condition.
Resetting the Brain
“Of all the chronic pain conditions, phantom-limb pain is one of the few that is pretty much a purely central pain phenomenon,” said Joel Castellanos, a pain physician at UCSD and sub-investigator on the trial as well as lead author of the 2020 review. “The pain comes from a dissonance between the lack of input from the nerves within the area of the brain that represents the area that’s no longer there,” Castellanos told Project CBD.
The way that psilocybin may help “bring the brain’s representation of the body back into alignment,” and thus snuff out the pain, is no different from how it can be used to help treat anxiety, depression, eating disorders, and other chronic neuropathic issues or “diseases of the central nervous system,” Castellanos said.
“Our brain gets in these firing patterns that are maladaptive and pathologic, and by using psychedelics as a reset button, it resets the brain’s ability to fire in a more healthy and efficient way,” he explained. “The longer patients are in these pathologic states, the more firm those neural pathways are … [T]he idea of something being able to reset those pathways is worth exploring further.”
Part 2: Migraines, Cluster Headaches & Psychedelics
Nate Seltenrich, Project CBD contributing writer, is the author of the column Bridging the Gap. An independent science journalist based in the San Francisco Bay Area, he covers a wide range of subjects, including environmental health, neuroscience, and pharmacology. © Copyright, Project CBD. May not be reprinted without permission.
Recommended Readings
Psychedelics for OCD
Why is psilocybin helpful for treating mood disorders? Is it the drug alone acting on the brain, or is it the subjective experience?
Psychedelic Research Targets Systemic Inflammation
Can scientists convert a super-hallucinogen into a wonder drug?
Psychedelics & Cannabis Therapeutics
High doses of THC are hallucinogenic, and microdosing LSD is a lot like CBD.