Flexibility is a physical state many of us strive for. Many times, while doing a forward bend in yoga class, I’ve glanced over with envy at a class companion with their head effortlessly positioned against their knees. Outside of the yoga studio (and in a doctor’s or physical therapist’s office), this might be categorised as “hypermobility.”
The most severe manifestation of hypermobility is a diagnostic symptom of the connective tissue disorder ehlers-danlos syndrome (EDS), a genetic condition that results in severe pain, regular joint dislocations, bowel complications, and chronic fatigue.
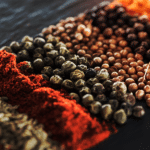
With their quality of life severely impaired, EDS patients often find themselves on a cocktail of prescription medication. Increasingly, however, cannabis is finding favor in the EDS community as a more effective and safe way to manage the complex symptoms they suffer.
In data published in the American Journal of Medical Genetics, 37% of the 500 EDS patients surveyed, said they used cannabis medicinally.1 Furthermore, of both the traditional and complementary therapies used by respondents, “marijuana was self-rated as most effective.”
What is Ehlers-Danlos Syndrome?
EDS is an inherited collection of connective tissue disorders caused by the abnormal structure or function of collagen, the main structural protein in the body. While officially classified as a rare disease, increasingly EDS is believed to be more prevalent than once thought, with one analysis of patients from Wales in the UK estimating that 1 in 500 of the local population are sufferers. Women are also more likely to be affected by EDS.2
While EDS is grouped into thirteen subtypes, the hypermobile EDS (hEDS) variant is the most common and is typified by loose, unstable joints that dislocate regularly, joint pain, stretchy skin, skin that bruises easily, digestive problems, and extreme fatigue. Comorbidities are frequent and include postural tachycardia syndrome (PoTS), an abnormal increase in heart rate and dizziness on standing; mast cell activation syndrome (MACS), resulting in allergic-like reactions triggered by normally unharmful substances; as well as fibromyalgia, and in women, endometriosis, the growth of uterine cells outside of the uterus.
In general terms, very little is known about hEDS. Despite its hereditary nature, no genetic test exists for diagnosis, and physicians generally struggle to manage patients’ symptoms, often resorting to long term prescriptions of heavy-duty opiates.
Lucy’s Story
This was the case for 21-year-old British EDS patient Lucy Stafford, who by the age of thirteen was taking opiates every day for the excruciating pain she was enduring.
“I just became basically a shell of myself who couldn’t really move and couldn’t study,” remembers Lucy. “I couldn’t attend school, I couldn’t do all the things that I should have been doing growing up. And instead, I got progressively sicker and started taking more and more and more medications to deal with a whole range of symptoms.”
Being whacked out on opioids made getting through schooling almost impossible and Lucy found herself failing almost all her classes.
“I just thought I was lazy and I just wasn’t capable of doing things,” she says thinking back.
As the medication got stronger (she was eventually put on fentanyl), Lucy’s condition worsened. A compromised digestive system wasn’t helped by the opiates she was prescribed. At her lowest point Lucy was in a wheelchair, being intravenously fed, was self-catheterizing to manage painful bladder spasms, and receiving daily nursing care.
“It scares me sometimes when I think about where I was headed,” admits Lucy, “We were at the point of looking at palliative care and making my life as comfortable as possible.”
Until cannabis entered her life.
Someone Who Can Do Things
It was Lucy’s consultant who first explored cannabis with her after a change in the law in 2018 meant medicinal cannabis could be legally prescribed in the UK. When his request was blocked, Lucy decided to source her own supply, eventually finding herself in a coffee shop in Amsterdam after catching the train there with her mom.
“It was like I was experiencing pain relief and symptom relief for the first time,” she remembers.
On her return to the UK, Lucy eventually got a legal prescription through a private clinic. This has enabled her to come off opiates completely. And in what could seem like a miraculous transformation, Lucy has gone from being wheelchair bound to walking 5km a day, roller skating, and swimming in the sea where she lives in Brighton.
“I’ve become so much stronger because I’ve been on cannabis,” says Lucy. “The best treatment for EDS is becoming as strong as possible, and I now do physio multiple times a day. Before cannabis, I just could not engage with that at all.”
Lucy, who is Advocacy Director at Patient-Led Engagement for Access, is now also better equipped to cope with her academic studies and is starting a degree in neuroscience in the autumn.
“I always just thought, ‘Oh, well, I’m someone with potential’. And now actually, I’m someone who can do things.”
Ellen’s Story
Unlike Lucy, Rhode Island resident Ellen Lenox Smith, 71, was not officially diagnosed with EDS until her fifties.
She had been hypermobile as a child and, with a host of sensitivities to food and medication, was said by her paediatrician to be allergic to her own body. That said, Ellen lived a normal life as a teacher, wife and mother, until her health fell apart in her early forties.
“I just was living with so much pain, neck pain, brain fog and couldn’t think straight,” recalls Ellen. “I had to have cheat sheets for kids in my classroom… I had to put down where they were sitting to remember their names, it was getting that severe.”
After multiple surgeries to ameliorate the pain she was experiencing from her regularly dislocating joints, like Lucy, Ellen eventually found herself in a wheelchair. And to top off her misery, an inability to metabolise most medications meant that she was forced to endure excruciating pain unmedicated.
In the end, it was a pain specialist who suggested cannabis.
“I sat there and laughed at him,” remembers Ellen who was totally unaware of how helpful cannabis might be for her condition.
Few Other Options
With few other options on the table, Ellen enlisted the help of a friend’s son who taught her how to turn the cannabis flowers she’d acquired off the black market into cannabis oil.
“I went to bed and next thing I know, it was morning,” she recollects, referring to the first night of decent sleep she had enjoyed in years.
As well as managing her pain, getting quality sleep has been one of the key benefits Ellen has experienced since taking her nightly teaspoon of home-made cannabis oil.
“What a gift it is to get deep, quality sleep. That really helped me to get stronger, too,” she explained.
And stronger Ellen has indeed become. At 71, her wheelchair days are well and truly behind her and she says she’s the best she’s ever felt. These days Ellen helps run the Rhode Island EDS support group, is on the board of the US Pain Foundation, and is committed to spreading the word amongst EDS patients about the therapeutic benefits of cannabis.
A Physician’s View
Canadian integrative and cannabinoid medicine physician Dr. Dani Gordon has seen first-hand the unique ability of cannabis in managing the pain, sleep, and chronic fatigue experienced by EDS patients.
“Medical cannabis can help with all three of these issues to a great degree,” says Dr. Gordon, “and is generally well tolerated (as long as you start with a very small dose especially with THC and go slowly titrating up). Many people with EDS have sensitivities to other medication and more side effects than average.”
Gordon regularly sees EDS patients successfully decrease their pill burden when using cannabis medicinally.
“Cannabis has such a huge impact on quality of life in EDS patients,” she says, “and can also reduce the amount of medications they need to feel well. It is very common to reduce other medications such as sleeping pills, pain pills, and even antidepressants and antianxiety medications once they are stable on medical cannabis. I wish more doctors and patients with EDS knew about this treatment as an option.”
While research into what role the endocannabinoid system may play in the development of EDS symptoms is lacking, Dr. Gordon suspects the interaction between phytocannabinoids and the ECS is worth exploring.
“Because cannabis impacts all of the most troublesome and difficult to treat associated symptoms in one go, it may work on regulating the ECS in some way,” she suggests. “There may be a possible connection between fascia dysfunction (which we see in EDS) and the endocannabinoid system activation and a possible link with inflammation regulation.”
A Call for More Research
In the cannabis world, it’s not unusual for drug development to be patient-led. Indeed, we’ve seen how with GW Pharma’s Sativex, multiple sclerosis (MS) patient experience inspired its development.
Curiously enough, figures from the UK’s MS Society suggest that the incidence of MS is somewhat similar to EDS. So it could be argued that there is as much to gain for pharmaceutical companies from investing in the development of a cannabis-based drug for ehlers-danlos syndrome as there has been for multiple sclerosis.
Dr. Gordon has her own theories why little interest has been shown by drug companies into EDS.
“As is the case with most conditions that affect women disproportionately,” she points out, “the research into women’s health and related conditions tends to lag behind.”
At the time of writing, Project CBD has been told that preliminary data is being gathered in a number of studies regarding the efficacy of cannabis in EDS patients. If the results reflect the overall positive anecdotal evidence so far, perhaps this will be enough to spur interest from the cannabis industry and bring about some much-needed clinical research.
A new case report, “Treating pain related to Ehlers-Danlos Syndrome with medical cannabis,” has just been published in BMJ Case Reports.
Lucy’s story is featured in the podcast Cannabis Voices hosted by Mary Biles. Mary Biles, a UK-based journalist, educator, and Project CBD contributing writer, is the author of The CBD Book (Harper Collins, UK). © Copyright, Project CBD. May not be reprinted without permission.
References
- Jessica S Demes et al. Use of complementary therapies for chronic pain management in patients with reported Ehlers-Danlos syndrome or hypermobility spectrum disorders. American Journal of Medical Genetics. Volume182, Issue11. November 2020 Pages 2611-2623
- Joanne C Demmler et al, Diagnosed prevalence of Ehlers-Danlos syndrome and hypermobility spectrum disorder in Wales, UK: a national electronic cohort study and case–control comparison. British Medical Journal. 2019; 9(11).
Recommended Readings
Cannabis & Chronic Fatigue Syndrome
What would you do if you were faced with the intractable symptoms of CFS? One woman’s experience.
Cannabis for Fibromyalgia
An Israeli observational study of 367 people using cannabis for fibromyalgia shows promising results.
Women Patient Cannabis Activists Fighting for Change
They saw a problem that needed a solution.