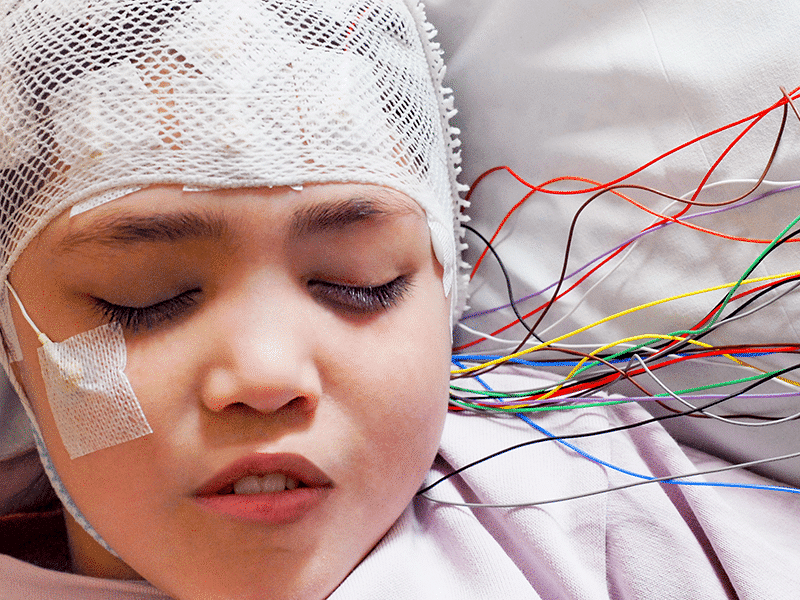
In countries around the world where medical cannabis is illegal, it’s generally assumed that a change in law will bring about safer access for patients. It’s often children with life-threatening seizures who are the catalysts for change. And yet in the UK, where cannabis was rescheduled in 2018, this extremely vulnerable patient group is struggling to find doctors willing to prescribe them medicinal cannabis.
Central to the problem lies a pitched battle between the professional body for pediatric neurologists, the British Pediatric Neurology Association (BPNA), and the parents desperate to get cannabis prescriptions for their children with intractable epilepsy.
Pediatric Neurology Association Is Hostile to Cannabis
While the BPNA doesn’t set the national regulations on prescribing medicinal cannabis to pediatric patients, they have made it all but impossible for clinicians to do so. Through a series of measures that include reporting a prescribing pediatrician to the General Medical Council (GMC) and the publication of guidance so hostile to cannabis that no pediatric neurologists will risk prescribing it to their patients, they have created a situation in the UK where only Epidiolex, GW Pharma’s approved oral CBD isolate medicine, can be prescribed.
However, for many children with intractable epilepsy, CBD alone is not enough, and only CBD-rich cannabis products containing small amounts of THC successfully control their seizures.
But with no doctors willing to prescribe the whole plant cannabis the parents believe their children need, the current deadlock represents an all-time low in proceedings. Prior to this, children had at least been able to get private prescriptions for unlicensed medical cannabis treatments through a handful of specialist clinicians prescribing out of private clinics (and thus far, only three children receive medical cannabis prescriptions through the National Health Service).
Putting Children at Risk?
Dr. Nathan Hasson, a pediatric rheumatologist, decided to train as a cannabis prescriber to better serve his young patients who presented with a variety of chronic pain conditions. When he was approached to start prescribing cannabis-based medicines for children with epilepsy, he felt sufficiently equipped due both to his background in general pediatrics and his training in medical cannabis.
With a shortage of pediatric prescribers, Dr. Hasson’s list quickly grew to more than fifty children with epilepsy whose seizures had failed to be controlled by a long list of anti-seizure medications. In all cases, the children’s pediatric neurologists were informed that cannabis was being used as an add-on treatment, however, according to Dr. Hasson the communication was only one way.
“They got all my letters, everything, so they were fully informed,” he recalls. “In fact, that’s how they all got together and complained because if I hadn’t written to them, and if the parents hadn’t told them, how would they have known about this?”
In total the BPNA complained twice about Dr. Hasson; the first time in a letter written by Professor Finbar O’Callaghan, then President of the BPNA, to the private hospital where Hasson had been seeing his patients. The second time, the BPNA reported Hasson directly to the General Medical Council (GMC), with Callaghan stating that “Dr. Hasson was potentially putting children at risk of harm with the way he practises outside his area of expertise and without consultation with the specialist doctors looking after these complex children” – a charge levelled based on GMC and NHS guidance for prescribing cannabis.
With his “fitness to practice” called in question and an investigation underway, Dr. Hasson was automatically dropped by all private medical insurers. As a result he lost 75% of his chronic pain patients (and income).
However, rather confusingly, the GMC did allow him to continue treating his epilepsy patients with medicinal cannabis. “Which already was a message in a way,” says Hasson. “If what I was doing was so awful, so bad and so wrong, how come the tribunal decided I could continue?”
Evidence of Benefit Not Harm
Which is exactly the conclusion reached by the GMC enquiry. They found that Dr. Hasson “provided adequate care to the families who consulted him, with evidence of benefit, and no evidence of harm.”
Not only that, they refuted the BPNA position that only pediatric neurologists should initiate treatment, stating it was “not supported by national guidance, and probably not in the best interests of children, as it may impede debate and research into the appropriate use of Cannibidiols (sic) in refractory epilepsy.”
In the context of some of the great medical cannabis breakthroughs of recent years we know this to be true. If Dr. Alan Shackelford, who is not a pediatric neurologist, hadn’t recommended that Charlotte Figi try CBD-rich cannabis to control her seizures, CBD and medical cannabis might not have gone mainstream when it did, and Epidiolex might never have existed.
However, rather than softening their resolve, losing the GMC case appears to have made the BPNA only dig deeper into the trenches. Recently they released their updated guidance to members on prescribing cannabis-based medicines to children with epilepsy, which takes an even more hard-line and unreasonable stance.
A sticking point for the BPNA is that the unlicensed whole plant cannabis-based products prescribed in private clinics haven’t been through the same gold standard randomised controlled trials as Epidiolex, and therefore are without sufficient data on both safety and efficacy.
Catch 22: A Lack of Randomised Controlled Trials
However, as stated in a recent critique by the Medical Cannabis Clinicians’ Society, the complex molecular makeup of most cannabis medicines does not lend itself well to randomised controlled trials, which typically focus on one compound with a single intended result. This sets up a catch-22 situation for cannabis in which real world evidence – such as the numerous observational studies coming out of the United States, Canada, Israel, and Australia – is ignored. As will data currently being gathered by Drug Science on the small cohort of children with intractable epilepsy receiving medical cannabis in the UK.
The BPNA also highlights the alleged risks posed by tetrahydrocanabinol (THC) to the developing brain citing studies examining the recreational use of high THC cannabis in adolescents. However, Project CBD maintains that it is both unscientific and unethical to use studies examining recreational consumption of street cannabis by teenagers as a criteria for ruling out the prescription of small amounts of THC for children with epilepsy. Furthermore, by denying them the seizure control that CBD-rich whole plant cannabis extracts, including THC, may bring, these children may not actually make it to the end of the year, let alone into adolescence.
Other Interests at Play?
But still, the BPNA’s position appears to be unwavering. This is perhaps not surprising when some of its key members such as Professor Callaghan and Professor Helen Cross were involved with the clinical trials of Epidiolex, and the BPNA itself receives donations from GW Pharma. Professor Callaghan, alongside his BPNA colleague Professor Martin Kirkpatrick, have also publicly written about their concerns that “children with epilepsy are at risk of being used as the ‘Trojan horse’ for the cannabis industry,” an opinion that clearly falls outside their professional remit as pediatric neurologists.
The BPNA guidance also instructs members not to privately prescribe medicinal cannabis in cases where parents cannot afford to pay for treatment on a long term basis, stating “we consider it unethical to initiate a treatment in private practice for which funding is not available in the longer term.” While it’s true that private medical cannabis prescriptions for children with epilepsy can cost upwards of $2000 a month, a sum unaffordable by most families with many resorting to remortgaging their homes or crowdfunding, should this be reason in itself to deny a cannabis prescription?
An Unethical Excuse, Says Dr. Bonni Goldstein
Matt Hughes, Co-Founder and Director of Medcan Support, an organisation supporting children with epilepsy seeking cannabis treatment in the UK, and father of Charlie who currently receives a private prescription for his intractable epilepsy, says a doctor’s choice to prescribe cannabis should not be based on a family’s finances.
“That’s down to the family to make the decision,” he insists. “That should have no basis on the clinical decision.”
Dr. Bonni Goldstein, a Los Angeles-area pediatrician who has treated many children with epilepsy in the United States over the years, firmly agrees with Hughes.
“It is not unethical to recommend something that the family may struggle to fund,” says Goldstein. “It is unethical to use this as an excuse. And it is unethical for the National Health Service (and insurance companies in the US) to choose not to help families pay for the cannabis medicine when it is helping the child, especially in cases where the cost of other medications that did not work are paid for by the NHS/insurance companies.”
“I have worked with hundreds of low socio-economic families who have found ways to pay for their child’s medicine,” she says. “There are also many cannabis companies that are willing to discount or donate cannabis products if a child is finding relief with their product.”
It would appear then that even in these extreme cases when children have unsuccessfully tried every available treatment and really are a point of no return, the BPNA prefers to ignore both the evidence from thousands of pediatric epilepsy patients around the world and the desperate pleas from parents, instead denying them the possibility of seeing whether unlicensed whole plant cannabis medicine might reduce their children’s seizures and give them some hope for the future.
Critical Situation
The result is that the UK currently finds itself in a critical situation in which the only remaining pediatric cannabis prescriber is no longer taking new patients. And thanks to the BPNA’s hostile guidance, which expressly advises members not to prescribe unlicensed cannabis medicines (contrary to recommendations from the National Institute of Health and Care Excellence), no new pediatricians, neurologist or otherwise, are prepared to put their head above the parapet.
And despite offers from the Medical Cannabis Clinicians Society to teach any pediatric doctor free of charge how to prescribe medical cannabis products, as well as providing ongoing mentoring and support, this impasse seems unlikely to change in the near future.
“The BPNA thinks they are protecting children, but it’s had the opposite impact,” says Matt Hughes. “It’s forcing families to seek cannabis from illicit sources or over the counter which inherently brings its own set of risks. Why the BPNA thinks this is safe practice is beyond belief.
“Instead children are left to suffer, families are left to suffer, and the devastating fact is children will die when maybe, just maybe, there is a medication which could have transformed their life.”
Mary Biles, a UK-based journalist, educator, and Project CBD contributing writer, is the author of The CBD Book (Harper Collins, UK). © Copyright, Project CBD. May not be reprinted without permission.
Recommended Readings
When CBD Isn’t Enough to Treat Epilepsy
Adult epileptics turn to THC when CBD falls short.
Slow Progress for Medical Cannabis in the UK
A year after cannabis rescheduling UK patients are still struggling with access.
What Causes Seizures?
Excerpted from “Foundational Concepts in Neuroscience: A Brain-Mind Odyssey” by David E. Presti, PhD.